Family Support
Inspiring Growth Starts With Compassionate Care
At Little Leaves, we believe in the power of families and are dedicated to providing the guidance and support needed to navigate an autism diagnosis with confidence and hope. Beyond therapy, we build connections among families, communities, and organizations passionate about supporting every child’s ability to thrive.
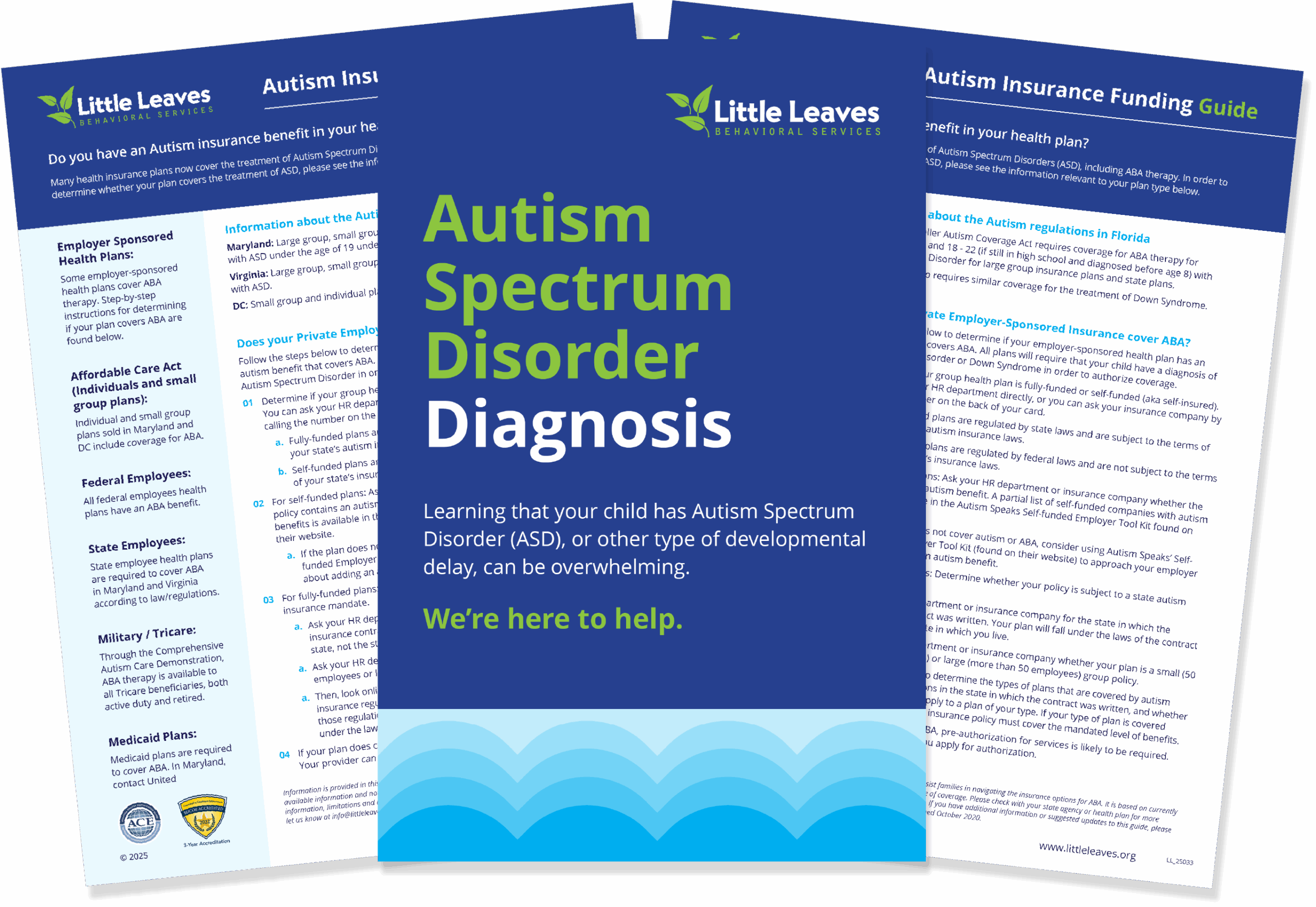
Family Resources
Our Process
At Little Leaves, we are committed to providing compassionate support to your child—and your family—every step of the way.
What to Expect on a Little Leaves Tour
Our centers are at the core of our program. Each of our locations is led by a highly credentialed and extremely compassionate Center Director who oversees the community within our walls. When you tour a Little Leaves center, not only will you get to put a face to our incredible team, but also see firsthand the vibrant, caring, and growth-oriented center your child will thrive in.
We Work with These Leading Insurance Providers